Is Inflammatory Bowel Disease Autoimmune?
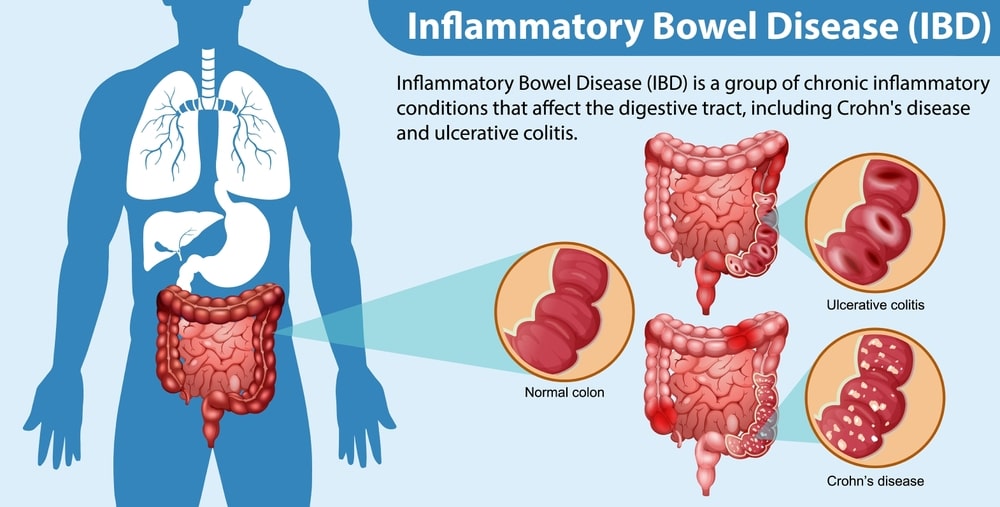
Inflammatory Bowel Disease (IBD) affects millions of people worldwide, causing chronic inflammation of the gastrointestinal tract and leading to a range of symptoms that significantly impact the quality of life. Among the questions frequently asked about IBD is whether it is an autoimmune condition.
In this blog post, we’ll delve into the complexities of IBD, exploring its connection to autoimmunity shedding light on the factors that contribute to its development, and discussing the question: Is inflammatory bowel disease autoimmune?
What causes Inflammatory Bowel Disease?
Here are some potential factors that may contribute to the development of IBD:
- Genetics: There is a strong genetic component to IBD. Individuals with a family history of the disease are at a higher risk of developing IBD themselves. Multiple genes have been implicated in IBD susceptibility, including those related to the immune system and the body’s ability to regulate inflammation.
- Immune System Dysfunction: In IBD, the immune system mistakenly attacks the gastrointestinal tract, leading to chronic inflammation. It’s believed that an abnormal immune response triggers inflammation in the digestive tract, although the exact mechanisms are not fully understood.
- Environmental Factors: Environmental factors, such as diet, smoking, stress, and exposure to certain pathogens or toxins, may contribute to the development or exacerbation of IBD.
- Dysbiosis of Gut Microbiota: The gut microbiota, which consists of trillions of bacteria and other microorganisms living in the gastrointestinal tract, play a crucial role in maintaining gut health and immune function.
- Intestinal Barrier Dysfunction: In individuals with IBD, there may be defects in the intestinal barrier that normally prevent harmful substances from crossing into the bloodstream. This increased intestinal permeability, also known as “leaky gut,” can lead to immune activation and inflammation in the gut mucosa.
- Autoimmune Response: Although IBD is not classified as a classical autoimmune disease like rheumatoid arthritis or lupus, it shares some similarities with autoimmune conditions. Hence, the question: Is inflammatory bowel disease autoimmune? can be cleared. In autoimmune diseases, the immune system mistakenly attacks the body’s tissues.
- Epigenetic Factors: Epigenetic modifications, which regulate gene expression without changing the underlying DNA sequence, may also play a role in IBD development. Environmental factors, such as diet and stress, can influence epigenetic factors too.
What are the symptoms of Inflammatory Bowel Disease?

Here are the common symptoms of IBD:
- Abdominal Pain and Cramping: Persistent or recurrent abdominal pain and cramping, often localized in the lower abdomen, are common symptoms of both Crohn’s disease and ulcerative colitis.
- Diarrhea: Chronic or intermittent diarrhea is a hallmark symptom of IBD. The stool may be loose, watery, or contain blood and mucus. In ulcerative colitis, diarrhea is often accompanied by an urgent need to defecate.
- Rectal Bleeding: Blood in the stool, which may appear as bright red or dark-colored blood.
- Weight Loss: Unintentional weight loss is common in individuals with active IBD, particularly during flare-ups. This can result from reduced appetite, malabsorption of nutrients, and increased metabolic demands due to inflammation.
- Fatigue: Chronic fatigue and weakness are common symptoms of IBD, often associated with the systemic inflammation and nutrient deficiencies that accompany the disease.
- Fever: Low-grade fever may occur.
- Rectal Urgency: Individuals with ulcerative colitis may experience a sudden and urgent need to have a bowel movement, often accompanied by an inability to control bowel movements (fecal incontinence).
- Anemia: Chronic intestinal bleeding in IBD can lead to iron deficiency anemia, characterized by fatigue, weakness, and pale skin. Anemia may also result from malabsorption of nutrients in the inflamed intestine.
- Loss of Appetite: Reduced appetite, nausea, and a feeling of fullness or bloating are common gastrointestinal symptoms of IBD, particularly during flare-ups.
- Joint Pain: Some individuals with IBD may experience joint pain and inflammation, a condition known as inflammatory arthritis or arthropathy.
- Skin Problems can also occur.
How to diagnose Inflammatory Bowel Disease?

Diagnosing inflammatory bowel disease (IBD), which includes conditions like Crohn’s disease and ulcerative colitis, typically involves a combination of medical history evaluation, physical examination, laboratory tests, imaging studies, and endoscopic procedures.
Here’s an overview of the diagnostic process for IBD:
- Medical History and Physical Examination
- Blood Tests
- Stool Studies
- Imaging Studies
- Endoscopic Procedures
- Capsule Endoscopy
- Other Tests: Depending on the clinical presentation and suspected complications, additional tests may be ordered, such as small bowel follow-through studies, nuclear medicine scans, or serological tests for specific antibodies associated with IBD.
Can Inflammatory Bowel Disease be cured?

No, there is no cure for IBD. There will be times when the illness is not active, known as remission periods. There is no cure, however, medications can lessen inflammation and lengthen and boost remission periods.
Dietary modifications may be useful in controlling your symptoms even though no particular diet has been demonstrated to prevent or treat IBD. It’s crucial to discuss diet modifications with your physician to ensure you’re getting the nutrients you require.
For example, the doctor might advise you to cut back on your intake of dairy products or fiber, based on your symptoms. Additionally, frequent, tiny meals could be easier to tolerate.
Learning how to handle stress is crucial for self-care because it can exacerbate symptoms. Making a list of the things that stress you out and deciding which ones to cut out of your daily schedule is one thing you might want to try.
Stopping the aberrant inflammation is the aim of medical treatment to allow intestinal tissue to recover. The symptoms of diarrhea and stomach ache should go away as it does.
The course of surgery for IBD varies depending on the condition. For example, because ulcerative colitis is confined to the colon, surgery can be used to treat the condition. After the colon is removed, the illness never reappears. Though certain operations may be done, Crohn’s disease cannot be cured by surgery.
In patients with Crohn’s disease, overstaging surgery may potentially exacerbate existing issues. The treatment modalities for IBD can be sought, but the question remains: Is inflammatory bowel disease autoimmune? Read the next section to clear the question.
Is Inflammatory Bowel Disease Autoimmune?

Yes, inflammatory bowel disease (IBD), which includes conditions like Crohn’s disease and ulcerative colitis, is considered to be autoimmune. Autoimmune diseases occur when the body’s immune system mistakenly attacks its tissues, leading to inflammation and tissue damage. In the case of IBD, the immune system targets the lining of the gastrointestinal tract, resulting in chronic inflammation and various gastrointestinal symptoms.
While the exact cause of IBD is not fully understood, it is believed to result from a combination of genetic, environmental, immune system, and lifestyle factors. Genetic predisposition plays a significant role, as individuals with a family history of IBD are at a higher risk of developing the condition themselves. Additionally, environmental factors such as diet, smoking, stress, and exposure to certain pathogens or toxins may trigger or exacerbate the autoimmune response in susceptible individuals.
In IBD, immune dysregulation leads to an abnormal inflammatory response in the gastrointestinal tract, characterized by the infiltration of immune cells and the release of pro-inflammatory cytokines. This chronic inflammation can damage the intestinal lining, leading to symptoms such as abdominal pain, diarrhea, rectal bleeding, and fatigue.
While IBD shares some similarities with other autoimmune diseases, such as rheumatoid arthritis and lupus, it also has distinct features and manifestations. Treatment for IBD aims to reduce inflammation, control symptoms, prevent complications, and improve quality of life. This may involve a combination of medications, lifestyle modifications, dietary changes, and, in some cases, surgery.
Overall, while IBD is considered to be autoimmune, the underlying mechanisms and triggers of the autoimmune response are complex and multifactorial. Further research is needed to better understand the pathogenesis of IBD and to develop more effective treatments for this chronic inflammatory condition. Hence, answering the question: Is inflammatory bowel disease autoimmune?
How to treat Inflammatory Bowel Disease?

Medications:
There are few medications to treat IBD, as the question is inflammatory bowel disease autoimmune? The management lies with the medications.
Anti-inflammatory drugs such as Corticosteroids (Prednisone), Mesalamine, and immunomodulators (e.g., Azathioprine, 6-Mercaptopurine) may be used to reduce inflammation and control symptoms during flare-ups.
Biologic therapies including anti-TNF agents (e.g., Infliximab, Adalimumab), anti-integrin agents (e.g., Vedolizumab), and anti-IL-12/23 agents (e.g., Ustekinumab), target specific proteins involved in the inflammatory response and are used to treat moderate to severe cases of IBD. Examples include Methotrexate, Cyclosporine, and Tacrolimus.
Antibiotics may be prescribed to treat bacterial overgrowth or infections that can exacerbate symptoms in individuals with IBD.
Nutritional Therapy:
Some individuals with IBD may benefit from dietary changes, such as avoiding trigger foods, following a low-residue diet during flare-ups, or incorporating specific nutrients or supplements (e.g., iron, vitamin B12) to address deficiencies.
Exclusive enteral nutrition (EEN) involves consuming a nutritionally complete liquid formula as the sole source of nutrition for some time. EEN has been shown to induce remission in some individuals with Crohn’s disease, particularly in children.
Lifestyle Modifications:
Smoking is a known risk factor for Crohn’s disease and can worsen symptoms in individuals with IBD. Quitting smoking may help improve disease outcomes. Stress management includes techniques such as mindfulness meditation, relaxation exercises, and counseling that may help manage stress and improve coping mechanisms.
Physical activity can help improve overall health and well-being in individuals with IBD. Consult with a healthcare provider to develop a safe and appropriate exercise plan.
Surgery:
Surgery may be necessary for individuals with severe complications of IBD, such as intestinal strictures, fistulas, abscesses, or perforations. Surgery may involve removing damaged portions of the intestine (resection), creating an ostomy, or repairing fistulas or other complications.
Monitoring and Follow-Up Care:
Regular monitoring and follow-up care with a gastroenterologist or healthcare provider experienced in managing IBD is essential for assessing disease activity, monitoring for complications, adjusting treatment as needed, and optimizing long-term outcomes.
FAQs:
Is diverticulitis an inflammatory bowel disease?
Yes, diverticulitis can be an inflammatory bowel disease. It shares radiological and clinical features.
Is irritable bowel syndrome the same as inflammatory bowel disease?
These are disorders of the digestive system that impact the stomach, intestines, and esophagus. IBS is a long-term condition characterized by a variety of symptoms. Conversely, inflammatory bowel disease (IBD) describes the persistent enlargement of the intestines.
Is colitis inflammatory bowel disease?
Yes, the term “inflammatory bowel disease” (IBD) refers to a group of two disorders that cause persistent inflammation of the gastrointestinal (GI) tract: Crohn’s disease and ulcerative colitis.
Can ultrasound detect inflammatory bowel disease?
Yes, transabdominal ultrasound can detect IBD. To be specific, the transabdominal type of USG can help with better detection.
Can you die from inflammatory bowel disease?
No, you can not die from IBD. One has to make a balance of living and diet to avoid worsening the condition. In the case of long-term or chronic conditions, it can be life-threatening. As the big question: is inflammatory bowel disease autoimmune? One can die from autoimmune diseases too if left untreated.